If you have a problem with your current breast implants, or just want to change the size, our experienced, board certified plastic surgeon is here to help. As a reputable San Francisco Bay Area and Walnut Creek breast implant revision specialist, Dr. Joseph A. Mele has performed hundreds of breast augmentation revision surgeries. Your breast augmentation results can be restored in a manner that is proportionate and natural-looking. You can anticipate excellent care and a comfortable experience while visiting our practice. Dr. Mele will determine if you are a good candidate for breast augmentation revision and explain the best method to achieve your goals during your in-person consultation appointment.
What Is Breast Augmentation Revision?
Breast augmentation revision surgery is a cosmetic plastic surgery procedure used to correct problems with breast implants and improve the results of breast augmentation, especially when complications arise. The outpatient procedure, also known as breast implant revision surgery or “breast implant exchange,” can improve the shape, feel, size and location of a woman’s breast implants should they deflate, become hard, or move to a less attractive position after breast augmentation.
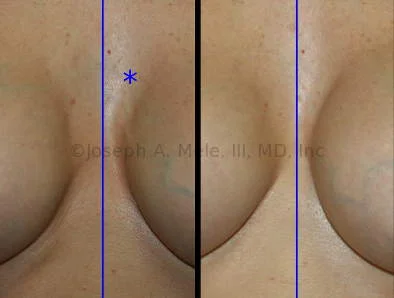
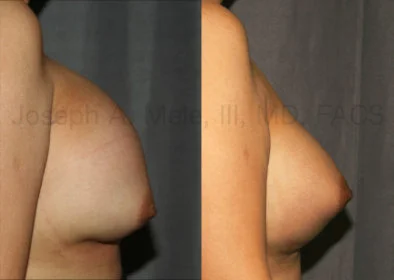
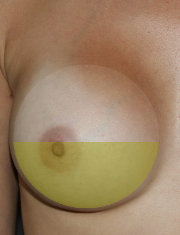
Breast Augmentation Revision Before and After Photos










































What Is Involved in Breast Augmentation Revision Surgery?
When performing breast augmentation revision, Dr. Mele first reviews and evaluates your breast surgery history. The size and shape of your breasts before breast surgery, your history of pregnancy and breastfeeding and how this changed your breasts, the previous surgical procedures and breast implants used, as well as how long it took the current problem to develop all influence your breast revision surgery. Once the problem is defined, a specific plan is developed to provide the safest and most predictable outcome. Options for breast revision surgery can fix problems with the breast implant’s pocket (the capsule) and correct problems with the breast implant itself. First, let’s review procedures that fix the capsule which holds the breast implant in place:
What Are the Procedures for Problems with the Breast Implant Pocket (Capsule)?
 The breast implant capsule is a pocket of scar tissue that naturally forms around the breast implants. The breast implant capsule is very important in maintaining the breast implants in their proper position. If the capsule is too big, the implant will move into the wrong position. It can end up too low, too medial (too close together) or too lateral (too far apart). If the breast capsule is too small, the result is a hard, tight breast implant, which is immobile, and it may end up stuck in a less ideal position. Capsular contracture occurs when the breast implant pocket constricts around the breast implant.
The breast implant capsule is a pocket of scar tissue that naturally forms around the breast implants. The breast implant capsule is very important in maintaining the breast implants in their proper position. If the capsule is too big, the implant will move into the wrong position. It can end up too low, too medial (too close together) or too lateral (too far apart). If the breast capsule is too small, the result is a hard, tight breast implant, which is immobile, and it may end up stuck in a less ideal position. Capsular contracture occurs when the breast implant pocket constricts around the breast implant.
A capsule that holds the breast implant in place, but is soft and not palpable, is the most common result. This is a grade I capsule. The second most common capsule is a grade II capsule, which still holds the breast implant in the proper position, but is slightly firm and resists movement. Grade III capsules are firm and may push the implant out of its ideal position. The least common capsule is a grade IV capsule. A grade IV capsule is like a grade III capsule, but is also tender. Grade III and IV capsules are the types that require surgical revision to restore a more aesthetic result.
Capsulotomy
A capsulotomy is the opening of the capsule (the pocket around the breast implant). It is used to expand the capsule in cases of breast implant malposition, when the breast implant is in the wrong position. A capsulotomy is used most often to lower the implant when the breast implant’s pocket is too high, or to bring the implants closer together when the pockets are too lateral. A capsulotomy may also be necessary as part of the repair for bottoming out, if the upper pocket has closed.
Capsulotomy can also be used for the treatment of capsular contracture in selective cases when the capsule is thin, but tight; however, a capsulectomy is often preferable. The differences between a capsulotomy and capsulectomy are described below, beginning with the two methods of capsulotomy: open and closed.
 Open Capsulotomy: An open capsulotomy is the surgical release of a breast implant’s capsule. This is usually performed in an operating room under anesthesia. An open capsulotomy provides the greatest safety and predictability of results. It also allows for other procedures to be performed at the same time, if necessary. Since the open capsulotomy is performed under direct vision, precise releases are possible, and the risk of bleeding and injury to the implant is reduced. Sometimes, simple capsulotomies can be performed under a local anesthetic with sedation. However, since this breast implant is exposed during an open capsulotomy, it should always be performed under sterile conditions.
Open Capsulotomy: An open capsulotomy is the surgical release of a breast implant’s capsule. This is usually performed in an operating room under anesthesia. An open capsulotomy provides the greatest safety and predictability of results. It also allows for other procedures to be performed at the same time, if necessary. Since the open capsulotomy is performed under direct vision, precise releases are possible, and the risk of bleeding and injury to the implant is reduced. Sometimes, simple capsulotomies can be performed under a local anesthetic with sedation. However, since this breast implant is exposed during an open capsulotomy, it should always be performed under sterile conditions.
- Closed Capsulotomy: A closed capsulotomy is performed by quickly and firmly squeezing or compressing the breast until the capsule around the implant tears. It is hard to predict where the capsule will tear. Moreover, if there is bleeding, the bleeding cannot be controlled like it can during an open capsulotomy. The closed capsulotomy is an older technique that has fallen out of favor because of the lack of precision and the increased risk of bleeding when compared to the open capsulotomy. A closed capsulotomy also has a higher risk of damaging the breast implant. If your breast implant deflates during a closed capsulotomy, your breast implant warranty may not cover you.
Capsulectomy
While a capsulotomy involves making cuts in the capsule to allow the pocket to expand, a capsulectomy is the removal of the capsule. During a complete capsulectomy, the entire lining of the breast implant pocket is removed. A partial capsulectomy, as the name suggests, is removal of a portion of the capsule. Complete capsulectomies are most often performed for the treatment of capsular contracture, when the capsule is thick. Capsular contracture is when the scar pocket around the breast implant becomes too tight. A breast pocket that is tight all around the implant can cause the breast to feel hard, and in some cases cause pain. A pocket that is tight in just one area can move the implant into a less desirable position (malposition). For example, a capsular contracture of the lower pole of the capsule will push the breast implant up. Depending on the problem, a complete or partial capsulectomy may be recommended.
 Complete Capsulectomy: A complete capsulectomy is the complete removal of the entire capsule, or pocket of scar tissue, that keeps the breast implant in its desired position. The most common reason for this is to remove a capsule that is too small and tight. Tight capsules squeeze the breast implants into a hard, spherical shape, which is not pretty. A soft, teardrop shape is usually preferred, and a capsulectomy allows breast tissue to drape more naturally around the implant. A new capsule will form, which is important to keep the breast implant from moving. The goal is that the new pocket will remain slightly larger than the breast implants and will provide a softer result that moves more like a natural breast.
Complete Capsulectomy: A complete capsulectomy is the complete removal of the entire capsule, or pocket of scar tissue, that keeps the breast implant in its desired position. The most common reason for this is to remove a capsule that is too small and tight. Tight capsules squeeze the breast implants into a hard, spherical shape, which is not pretty. A soft, teardrop shape is usually preferred, and a capsulectomy allows breast tissue to drape more naturally around the implant. A new capsule will form, which is important to keep the breast implant from moving. The goal is that the new pocket will remain slightly larger than the breast implants and will provide a softer result that moves more like a natural breast.
 Partial Capsulectomy: A partial capsulectomy is the selective removal of a portion of the capsule. It is often performed to reposition a breast implant when a capsulotomy is insufficient, or when only a portion of the capsule is too tight. A partial capsulectomy can range from removing a strip of capsule to a near-complete capsulectomy. Near-complete capsulectomies include removal of almost all of the capsule. Reasons for leaving a portion of the capsule may include not wanting to further reduce thin coverage over the breast implant, or leaving a patch of very adherent capsule behind the implant if removal is more likely to cause injury or bleeding rather than provide a benefit.
Partial Capsulectomy: A partial capsulectomy is the selective removal of a portion of the capsule. It is often performed to reposition a breast implant when a capsulotomy is insufficient, or when only a portion of the capsule is too tight. A partial capsulectomy can range from removing a strip of capsule to a near-complete capsulectomy. Near-complete capsulectomies include removal of almost all of the capsule. Reasons for leaving a portion of the capsule may include not wanting to further reduce thin coverage over the breast implant, or leaving a patch of very adherent capsule behind the implant if removal is more likely to cause injury or bleeding rather than provide a benefit.
Capsulorrhaphy
Capsulorrhaphy is the surgical term for tightening the capsule. A capsulorrhaphy is performed when the capsule is too big, and is often used to correct breast implant malposition. Signs of the capsule being too large include:
- Breast implants that fall to the sides of the chest, creating a large gap between the breasts
- Breast implants that cross the midline or meet in the middle (symmastia, “uni-boob” or “bread-loafing”)
- Breast implants that are too low (bottoming out)
By reducing the pocket where it is too big, the position of the breast implant can be improved, and a more attractive result is possible. In cases where the capsule is thin, or the repair is tenuous, a patch may be used to reinforce the capsulorrhaphy. More details of the main types of capsulorrhaphies and the materials available for reinforcement are discussed below.
Direct Capsule Modification
 Lateral Capsulorrhaphy (Wide Gap Repair): Breast implants should naturally fall to the side when we lay down, but sometimes, the amount of lateral movement is excessive. This is more common in women who continue to sleep on their stomachs after breast augmentation. With time, the constant pressure displaces the breast implants outward and causes the central portion of the breast implant pocket to close. Surgical improvement is often possible by reopening the inner aspect of the pocket (medial capsulotomy) and closing the lateral aspect of the pocket (lateral capsulorrhaphy). Outward movement of the breast implants is enhanced by breast implants that are too large or too wide for your chest, and anatomic factors like chest tissue that is too thin to support the breast implant and rib shape that is prominent centrally and angles laterally.
Lateral Capsulorrhaphy (Wide Gap Repair): Breast implants should naturally fall to the side when we lay down, but sometimes, the amount of lateral movement is excessive. This is more common in women who continue to sleep on their stomachs after breast augmentation. With time, the constant pressure displaces the breast implants outward and causes the central portion of the breast implant pocket to close. Surgical improvement is often possible by reopening the inner aspect of the pocket (medial capsulotomy) and closing the lateral aspect of the pocket (lateral capsulorrhaphy). Outward movement of the breast implants is enhanced by breast implants that are too large or too wide for your chest, and anatomic factors like chest tissue that is too thin to support the breast implant and rib shape that is prominent centrally and angles laterally.
 Medial Capsulorrhaphy (Symmastia Repair): Breast implants that are too close together can lift the skin between the implants and merge into one large breast. This is termed “symmastia,” but is also known as “uni-boob” and “bread-loafing.” Breast implant revision surgery is used to re-establish the separation between the two breasts. A medial capsulorrhaphy is used to close the inner portion of the breast implant capsule to prevent the breast implants from getting too close together. When the breast tissue is weak, the capsulorrhaphy may need to be reinforced with a patch, as described below. In other cases, a new pocket needs to be created. This can be done by moving breast implants that are in front of the muscle to behind the muscle. If your breast implants are already behind the muscle, a pocket can often be created behind the current capsule. This later procedure goes by the name Neopocket Formation. Since symmastia is most commonly seen in women with tight skin and large, often high-profile breast implants, changing to smaller or lower profile breast implants can help decrease the risk of recurrence.
Medial Capsulorrhaphy (Symmastia Repair): Breast implants that are too close together can lift the skin between the implants and merge into one large breast. This is termed “symmastia,” but is also known as “uni-boob” and “bread-loafing.” Breast implant revision surgery is used to re-establish the separation between the two breasts. A medial capsulorrhaphy is used to close the inner portion of the breast implant capsule to prevent the breast implants from getting too close together. When the breast tissue is weak, the capsulorrhaphy may need to be reinforced with a patch, as described below. In other cases, a new pocket needs to be created. This can be done by moving breast implants that are in front of the muscle to behind the muscle. If your breast implants are already behind the muscle, a pocket can often be created behind the current capsule. This later procedure goes by the name Neopocket Formation. Since symmastia is most commonly seen in women with tight skin and large, often high-profile breast implants, changing to smaller or lower profile breast implants can help decrease the risk of recurrence.
 Inferior Capsulorrhaphy (Bottoming-Out Repair): When the breast implants fall below the nipple this is called “bottoming out.” When they fall below the crease under the breast (the inframammary fold or IMF), it can cause a “double bubble.” Reducing the lower half of the breast implant capsule is often part of the repair of implant malposition when the breast implant is too low. Closing the lower pocket supports the implant higher on the chest, and prevents the implant from sliding too low. If the problem is that the breast implant is too large for the breast skin to support, reduction in the breast implant volume may also be recommended. If the breast implant is in a good position, but the breast itself has fallen, a breast lift may be a better option. In some cases, the inferior capsulorrhaphy repair is reinforced with a patch, as described in the next section.
Inferior Capsulorrhaphy (Bottoming-Out Repair): When the breast implants fall below the nipple this is called “bottoming out.” When they fall below the crease under the breast (the inframammary fold or IMF), it can cause a “double bubble.” Reducing the lower half of the breast implant capsule is often part of the repair of implant malposition when the breast implant is too low. Closing the lower pocket supports the implant higher on the chest, and prevents the implant from sliding too low. If the problem is that the breast implant is too large for the breast skin to support, reduction in the breast implant volume may also be recommended. If the breast implant is in a good position, but the breast itself has fallen, a breast lift may be a better option. In some cases, the inferior capsulorrhaphy repair is reinforced with a patch, as described in the next section.
Augmented Capsule Modification
 Acellular Dermal Matrix (ADM) are materials that can be used to reinforce the breast implant pocket and to anchor the muscles used to cover the breast implant. All ADMs are processed skin. Some are derived from human donors, like Alloderm® (LifeCell™), FlexHD® (Ethicon), DermaMatrix™ (Synthes), and AlloMax™ (Bard®). Others are made from non-human sources like pig skin – Strattice™ (LifeCell™), and cow skin – SurgiMend® (TEI Biosciences). ADMs have been used for breast surgery since 2001, and have become increasingly common in breast reconstruction and complicated breast revision surgeries. They have the appearance and handling characteristics of soft, white leather, and can be ordered in varying thickness.
Acellular Dermal Matrix (ADM) are materials that can be used to reinforce the breast implant pocket and to anchor the muscles used to cover the breast implant. All ADMs are processed skin. Some are derived from human donors, like Alloderm® (LifeCell™), FlexHD® (Ethicon), DermaMatrix™ (Synthes), and AlloMax™ (Bard®). Others are made from non-human sources like pig skin – Strattice™ (LifeCell™), and cow skin – SurgiMend® (TEI Biosciences). ADMs have been used for breast surgery since 2001, and have become increasingly common in breast reconstruction and complicated breast revision surgeries. They have the appearance and handling characteristics of soft, white leather, and can be ordered in varying thickness.
- SERI® (Sofregen) is an absorbable silk surgical scaffold. It is not derived from animal skin. It is a knitted, multifilament, purified silk that slowly absorbs, leaving behind a supportive collagen matrix. It has possible advantages over dermally derived products, including a lower cost and potentially less sagging over time. Per the FDA website, the SERI® Surgical Scaffold was cleared under 510(K) Number K123128 with the following indications: for use as a transitory scaffold for soft tissue support and repair to reinforce deficiencies where weakness or voids exist that require the addition of material to obtain the desired surgical outcome. This includes reinforcement of soft tissue in plastic and reconstructive surgery, and general soft tissue reconstruction. While SERI® and others that are FDA-approved for reinforcement of soft tissue are used for breast reconstruction, it is important to note that this is still an off-label use. Surgical mesh has not been FDA-cleared or approved specifically for use in breast reconstruction using a tissue expander or implant. The concern is that if SERI®, or any ADM, is placed on the implant, only the other side of the product is in contact with soft tissue, and it may be less likely to integrate. SERI® can be used outside the breast implant’s capsule to reinforce soft tissue. Examples include reinforcing the repair of symmastia or reinforcing the muscle repair in cases where the pectoralis muscle has been widely separated from its insertion on the ribs or sternum. Keeping the product outside the capsule isolates the SERI® patch from the implant or expander, promotes better ingrowth of the product, and is more in keeping with its approved use.
What Are the Procedures for Problems with Breast Implants?
Sometimes the capsule is perfect, and the problem is the breast implant itself. Breast implants are not lifetime devices. That is to say, the lifespan of your breast implant may be shorter than yours. Breast implants can wear out or get damaged and may require maintenance from time to time. Changing size is one of the most common reasons for breast implant revision surgery. A change in size may be desired even when there is nothing wrong with the breast implant or the breast capsule. Sometimes breast augmentation is no longer desired. The normal increase in weight that occurs with aging may lead to an increase in breast size and a desire to have your breast implants removed. Breast implant replacement and breast implant removal are discussed further below.
Breast Implant Replacement – Breast Implant Exchange
Breast implant replacement involves a few simple steps. The previous incision can often be used. The existing breast implants are removed. The capsule is inspected, and often modified, to accommodate the new breast implants. Malposition of the previous breast implants can often be addressed before the new breast implants are inserted. Recovery is usually just a few days, and the postoperative pain is often significantly less when compared to the recovery after primary breast augmentation.
Reasons for breast implant replacement include:
- Changing Breast Implant Size: The most common reason for breast implant replacement is to change size. While increasing the volume of the breasts is most common, decreasing the size of the breasts is also possible. The surgery to increase the size of the breast implants is usually simpler, faster, and less painful than the original breast augmentation. Oftentimes, enlarging the breast pocket (a capsulotomy) is required to make room for the larger breast implants. When reducing the size of breast implants, the breast pocket is usually reduced with a capsulorrhaphy. For large decreases in volume, a breast lift may be needed to support the breasts in a youthful position.
- Changing Breast Implant Type: Another reason to change breast implants is to switch the type or style of the breast implants. Breast implants may be changed from saline-filled to silicone gel-filled or vice-versa. Older silicone breast implants may be changed to the newer “Gummy Bear” breast implants to decrease the risk of gel migration in case of a leak. At times, changing the profile or shape of the breast implant may provide a better breast shape, and this is another reason for breast implant replacement surgery.
- Breast Implant Deflation: A non-elective reason for breast implant replacement is breast implant deflation. When a breast implant leaks, it should be removed. Most often, the defective breast implant is immediately replaced with a new implant. If you have a deflated breast implant, be certain to check your breast implant warranty to see if you are eligible for financial assistance or a free replacement breast implant. Breast implant warranty information is available below, but be certain to check with your manufacturer for the latest details, as coverage changes from time to time.
Breast Implant Removal
Breast implant removal may be elective or emergent. Elective reasons for breast implant removal include:
- No Longer Desiring Breast Augmentation: Sometimes, the desire for breast augmentation fades. If your breast implants are relatively small, and your breast volume is good, the result of breast implant removal is often good, as well. On the other hand, if you have large breast implants and very little breast tissue, skin laxity can be a problem, and a mastopexy (breast lift) may be needed.
- Breasts Got Bigger: After pregnancy or if you gain weight, sometimes the natural breast tissue enlarges. Removing the breast implants may be enough to reduce your breast volume back to a more comfortable size without the need for a breast reduction or breast lift.
- Changes in Lifestyle: Sometimes, changes in lifestyle or activity can change the way we feel about our breasts. Elective breast implant removal can restore a slimmer, more athletic build.
Non-elective reasons for breast implant removal include:
- Exposure of the Breast Implant: Injury or inadequate soft tissue coverage can lead to exposure of the breast implant. This is most common after breast reconstruction, especially after radiation, but can rarely occur in otherwise healthy women. Once an implant has been exposed, it is contaminated and needs to be removed.
- Infection: Infection around breast implants is rare. The initial treatment for an infection around a breast implant is antibiotics. In about half the cases of infection, however, antibiotics alone are not enough, and the breast implant will need to be removed in order to get the infection to clear.
- Failure of the Breast Implant: Sometimes, breast implants break. A leaking breast implant should be removed. Since there is rarely exposure or infection associated with a breast implant deflation, the implant is usually replaced during the same operation.
Breast Implant Warranties
All three US-based breast implant manufacturers have a warranty program for their breast implants. Natrelle® (Allergan), Mentor® (Johnson & Johnson) and Sientra® (Silimed) all have generous warranties, including lifetime breast implant replacement. If your breast implant ever leaks, a new one will be supplied for replacement absolutely free. If a breast implant leaks within ten years of your initial breast augmentation, financial assistance may be available to help pay the surgical costs associated with breast implant replacement. Warranty information is available below via the supplied links. For the latest details, please consult with your plastic surgeon or check your breast implant manufacturer’s website. Breast implant warranties are frequently updated.
Natrelle® Breast Implants (Allergan)
- Allergan – Natrelle® ConfidencePlus® Breast Implant Warranty
- Allergan – Natrelle® ConfidencePlus® Premier Breast Implant Warranty
Mentor® Breast Implants (Johnson & Johnson)

- Mentor® – Saline Breast Standard Advantage and Advanced Advantage Breast Implant Warranties
- Mentor® – MemoryGel® (Silicone Gel) Breast Implant Warranty
Sientra® Breast Implants (Silimed)

Recovery from Breast Augmentation Revision – What to Expect
Breast augmentation revision surgery encompasses a large variety of procedures, so the recovery is variable. In general, recovery from most revision surgery is easier than the recovery after the original breast augmentation.
For revisions when minimal capsular modification is necessary, like replacing a deflated breast implant or the correction of mild superior malposition, recovery is a few days. For revisions encompassing complete reconstruction of the capsule (like symmastia), severe bottoming out or lateral displacement, repair, and reinforcement of the capsule, recovery may take a few weeks.
Be certain to ask your doctor about the recovery for your specific procedure. Pain control, activities, and weight restrictions should be outlined before surgery so that you can plan accordingly and get the best results.
Breast Augmentation Revision Follow-Up
Like all elective cosmetic plastic surgery, follow-up appointments are an important part of obtaining the best results. From forming the proper breast implant capsule to scar modification, many aspects of your healing can be modified after surgery. While the proper surgical plan and operative technique can set the stage for a great result, follow-up is important for both promoting the best results and for preventing additional problems and complications. We expect to see you in our office for follow-up visits many times after your breast augmentation revision procedure. Initially, your follow-up appointments will be frequent to closely monitor your progress and will be adjusted, as necessary, as you continue to heal. Dr. Mele likes to follow his patients closely to assure the best possible results.
How Much Does Breast Revision Cost?
Breast augmentation revision surgery encompasses many procedures, so there is a wide range of costs. After your consultation, you will be supplied with an operative plan and an estimated cost.
The cost of a procedure is influenced by many factors. Simple procedures tend to take less time and cost less. Complicated procedures take longer and cost more. The operating room and anesthesia charges are based directly on the duration of the surgery, while the surgeon’s professional fee is usually based on the complexity of the operation.
The use of implants and mesh also increases the cost. These are fixed costs and are passed on to the patient. Breast implants often have a warranty, and in cases of breast implant rupture, the implants are often supplied by the manufacturers for free. Be certain to check your breast implant manufacturer’s warranty as they change every few years.
Incidentals such as prescription drugs, dressings, scar creams, and garments may be required. Be certain to ask your plastic surgeon which, if any, are covered in the cost of the procedure.
Contact Our Breast Augmentation Revision Specialist
If you have a problem with your current breast augmentation and are looking to enhance your results, it is important to seek the expertise of a board-certified plastic surgeon such as Joseph A. Mele, MD, FACS. Individuals who decide to undergo a breast augmentation revision with Dr. Mele may anticipate being well cared for in a comfortable and compassionate setting.
Dr. Mele and his staff will do everything they can to schedule convenient appointments, attentively listen to your desires, and fully address your cosmetic plastic surgery concerns.
Dr. Mele will further discuss enhancement options with you during your personal consultation. You will want to bring any information you have about your current breast implants, and obtain your operative reports from previous surgeries, so that Dr. Mele can review them with you. Breast augmentation revision surgery can be combined with body contouring procedures such as breast lift surgery (‘mastopexy’) or tummy tuck surgery (“abdominoplasty”), or other breast and belly enhancement procedures, as part of a Mommy Makeover, which is designed to help a woman regain her pre-pregnancy body.
To learn more about breast augmentation revision surgery, or to schedule an initial consultation with Dr. Mele, please contact us today.